Schedule a quick demo to learn about the cost saving benefits

Download a Case Study with ROI metrics

Cost-Per-Patient Optimization Tools
Hospitals across the US are countering the negative effects of rising inflation by saving millions of dollars each year by reducing physician controlled orders and managing length of stay. And the solution is quick to implement, easy to use, and has a documented ROI. IllumiCare’s patented Smart Ribbon technology takes a multi-pronged approach to addressing overutilization by displaying actionable data, when contextually appropriate, within the clinical workflow by hovering unobtrusively over the EMR screen.
Real savings are achieved through your ability to:
- Expose lower cost opportunities for meds, labs and rads;
- Reduce length of stay by displaying clinical barriers to discharge;
- Compare spending per admission among clinicians in the same specialty;
- Notify providers of the amount of time a patient has been on obs status;
- Provide a high-level view of the financial and clinical impact of lab orders;
- And display high-priority clinical posts relevant to healthcare personnel.
Check out the benefits and features in the drop downs below, click on the banner above to request a one-page case study of an actual client with a similarly sized facility, or schedule a short demo.
-
Overview
-
Screenshot
-
Video - Stewardship Overview
-
Video - Training
-
FAQs
REAL-TIME COST TRANSPARENCY
We ask for “value-based care” but how are providers supposed to make value judgments if they don’t know what things cost? The Stewardship App teaches and reinforces a value mindset by exposing real hospital costs to providers and nudging in their clinical workflow when lower cost opportunities exist, supplemented with clinical guidance and citations. The result is an average of $86+ per admission in hard-dollar savings, adding up to millions of dollars.
ATTRIBUTED TO THE RESPONSIBLE PROVIDER
The app uses your own wholesale acquisition cost for medicines and your direct, variable cost accounting data for labs to give a true representation to providers of what things cost. More importantly, we know the cost of every order, by every provider, the provider specialty and the patient’s acuity. From that, we understand variation in practice patterns among similar providers. We use machine learning to turn our understanding of each provider’s practice tendencies into personalized contextual education. Content is delivered to the right provider at the right time…but not too often.

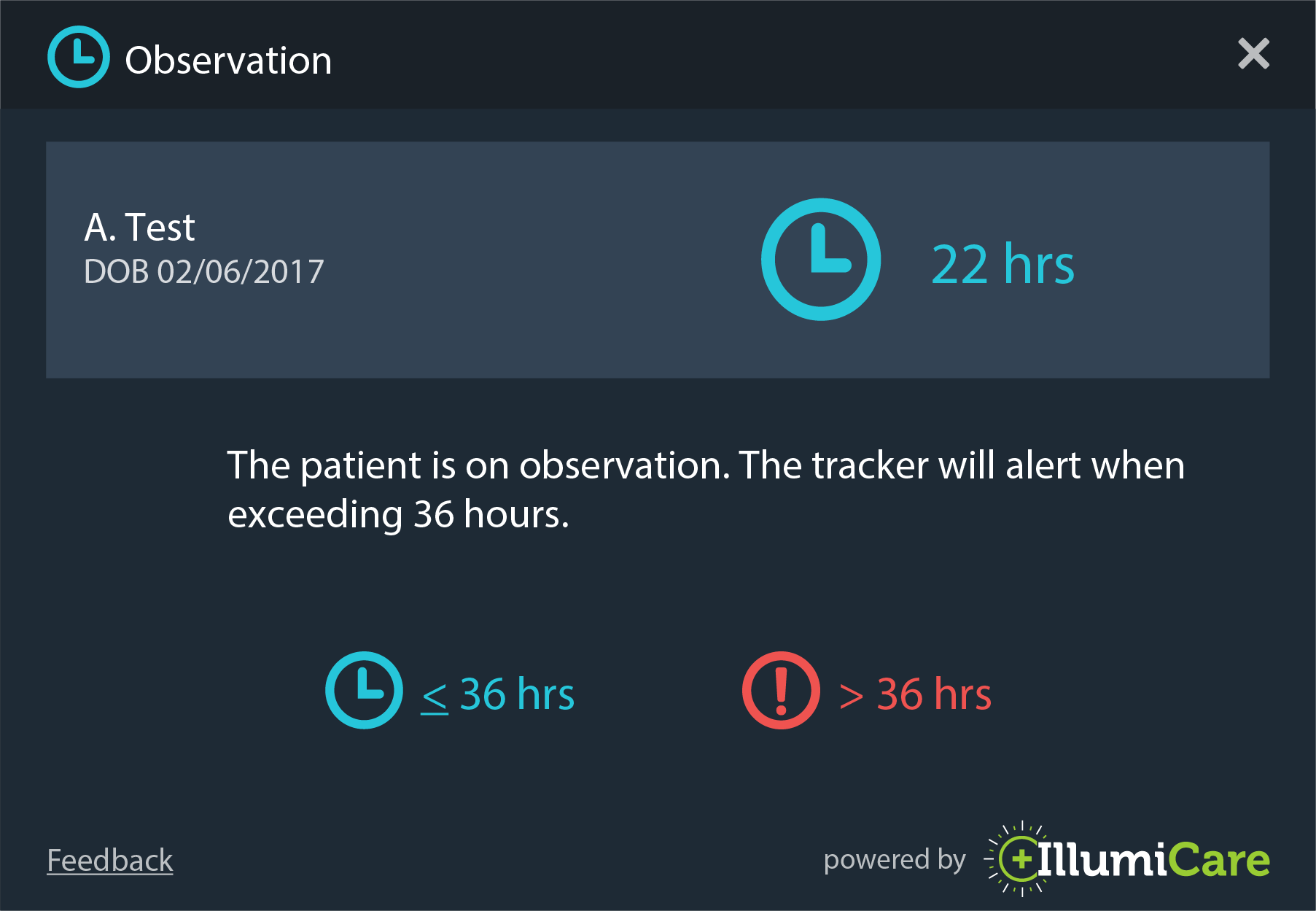
What timers can be seen and what are they?
The following timers will be displayed based on the patient’s current patient class/type: Inpatient (Length of Stay based on patient days), Observation (length of time patient has been on observation status), and ED (time since the patient checked in).
How is C Diff % Risk calculated?
This is the iatrogenic C Diff risk, related to current active scheduled medications. Our calculations consider the specific risk that exists for each specific antibiotic and/or protein pump inhibitor as well as the compounding affect that occurs when the patient has been prescribed multiple antibiotics and/or PPIs concurrently.
How is Fall Risk calculated?
The fall risk represents the relative risk of falling based on the intake of scheduled sedatives and opioids if aged 65 or greater. Please note, this calculation only considers current scheduled medications. Medications prescribed as PRN are not currently factored in as a part of this fall risk calculation.
What lab costs are displayed in the Stewardship app?
Lab costs derive from the Medicare Allowable Rate. The costs are not charges or what the patient pays.
How is blood loss calculated?
IllumiCare calculates the total phlebotomy blood draw that occurs based on the average amount of blood that must be drawn for each test ordered. We do consider other factors in our calculation, for example, when multiple lab tests are ordered at the same time, they may leverage the same blood draw.
What Rad costs are displayed in the Stewardship app?
Rad costs derive from the Medicare Allowable Rate. The costs are not charges or what the patient pays.
-
Overview
-
Screenshot
-
Video
-
FAQs
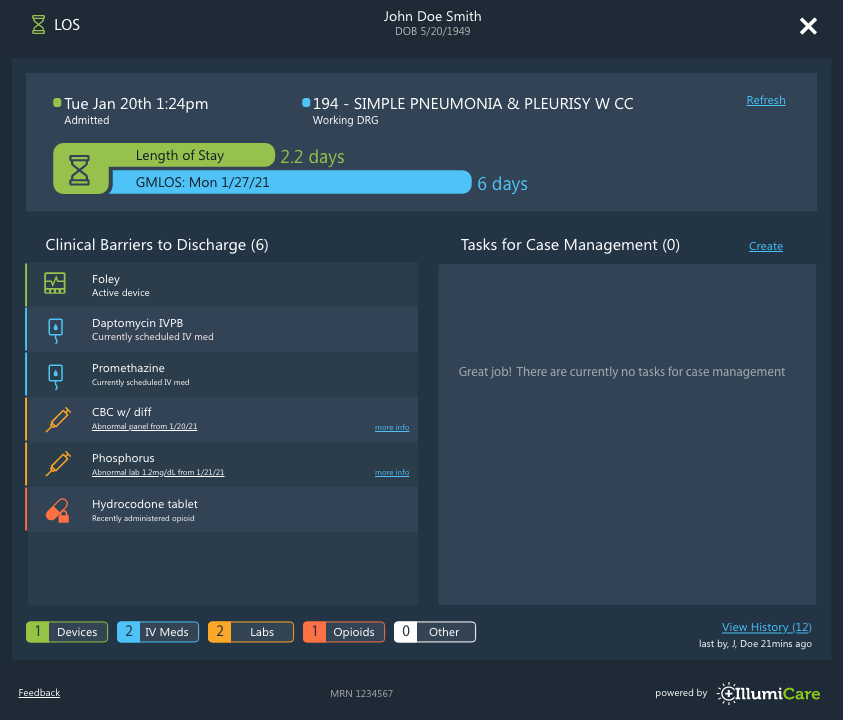
REMOVE BARRIERS TO DISCHARGE
Reduction in the number of inpatient days results in decreased risk of infection and medication side effects and increased hospital profit with more efficient bed management. But, with providers facing a mental deluge every day, opportunities for an earlier discharge can slip. The LOS App compiles the clinical barriers to discharge, making it easy for providers to tick down the list if a patient is ready to go. By organizing and front-facing this key information, we make it easier for providers to do what’s in the best interest of the patient and hospital.
STAY ON TRACK FOR GMLOS
The LOS App displays the current length of stay versus the CMS Geometric Mean Length of Stay (GMLOS) and number of clinical barriers to discharge right on the app icon. The app color even changes as patients approach or exceed GMLOS. These give front-facing visual clues when providers should start planning for discharge. Clinicians can even add tasks for case management that are pertinent to discharge or readmission (without making them part of the formal record). Case Managers see the same app when rounding and can acknowledge tasks as completed. This also facilitates multi-disciplinary rounds. Anyone on the care team can see the history of app views and changes.
LOS Screen
What is the LOS App?
The LOS app displays key data elements that need to be addressed to reduce a patient’s length of stay.
What does LOS stand for?
LOS stands for Length of Stay; LOS number in this app is displayed in decimal to tenths place to give user accurate count of the number of days the patient has been admitted.
What does GMLOS stand for?
GMLOS stands for Geometric Mean Length of Stay, which is based off of the patient’s diagnosis related group (DRG), which is a system of grouping together clinically similar patients.
What is the View History button for?
View History button displays various user actions within the app and the time these actions occurred. These may be helpful to users who are interesting in knowing who is viewing the app or creating, editing, and completing barriers.
What does the Refresh button do?
Refreshing the app merely reloads the app and can be used to view changes other users have made since you last opened the app.
What are Clinical Barriers?
Clinical Barriers are any barriers that prevent the clinician to discharge the patient.
Example of Clinical barriers are:
- Opioids taken within last 24 hours - if the patient has been given opioids then he/she cannot be discharged home without proper med management.
- IV medications still being administered - if the patient is on IV Meds then can only be discharged to an SNF otherwise they cannot be discharged.
- Abnormal lab tests within the last 24 hours - if the results for the labs drawn for the patient are abnormal then the patient can’t be discharged.
- Peripheral devices in use - if the patient is on any of the devices (ex. Foley, Central line, Ventilator, Oxygen, etc.) then the devices have to be removed before the patient is discharged.
-
Overview
-
Screenshot
-
Video
-
FAQs
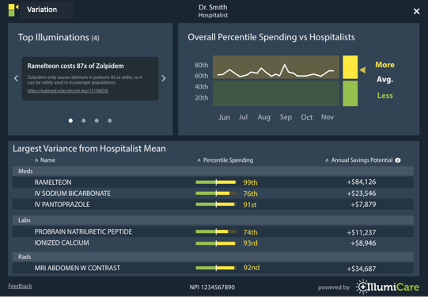
COMPARE SPENDING
The Variations App allows a provider to compare on a DRG-adjusted basis his/her real-time spending per admission with their specific sub group, and highlights specific opportunities for improvement. A physician’s moving average is also provided.
HOW IS MY CARE RISK ADJUSTED?
IllumiCare creates cohort of patients based upon their final DRG. This cohort methodology allows IllumiCare to compare the costs of patients within DRG groups such that the cohorts have similar acuity. Creating cohorts with homogeneous acuity and specialty provides a stable basis for comparing physician resource utilization.
HOW DO I KNOW WHAT IS GOOD?
A provider’s overall percentile, when compared with their peers, is presented in a run chart graph widget. The area in green means that cost outcomes were above the median of the group, while red means that costs were below the median. The higher the percentile, the lower the overall costs.
WHERE DOES MY VARIABILITY COME FROM?
IllumiCare details specific areas where a provider uses more resources than their peers in the incremental breakout of resource utilization. Areas such as medication category, imaging modality and lab are all detailed to show overall incremental cost difference over the last two months.
Coming Soon!
Who are my peers and how is my care risk adjusted?
Peer groups are established working with your administration and medical staff office. Utilizing your credentialed specialty and your patient care patterns your peer group was selected to ensure a homogeneous cohort. IllumiCare creates cohort of patients based upon their final DRG. This cohort methodology allows IllumiCare to compare the costs of patients within DRG groups such that the cohorts have similar acuity. Creating cohorts with homogeneous acuity and specialty provides a stable basis for comparing physician resource utilization.
How do I know what’s good?
The providers overall percentile, when compared with their peers, is presented in run chart graph widget. The area in green means that your cost outcomes were above the median of the group and the are in red means that your costs were below the median. The higher your percentile the lower your overall costs.
How do I see where my variability comes from?
IllumiCare details specific areas where a provider uses more resources than their peers in the incremental breakout of resource utilization. Areas such as medication category, imaging modality and lab are all detailed to show your overall incremental cost difference over the last two months. Selecting a category with a cost delta provides a view of the specific medications where your resource utilization differs from your peers.
-
Overview
-
Screenshot
-
Video
-
FAQs
LAB COSTS
The ARUP App, powered by the IllumiCare Smart Ribbon, provides clinicians with a high-level view of the financial and clinical impact of lab orders including access to the ARUP Consult® web tool and ARUP Frequency Algorithms. We never tell the provider not to order another test. We just provide them with the context they need to make a proper judgment about whether the utility of that next test is worth the cost and patient risk.
LABS ORDERED BY COST AND DATE
Labs ordered in the current admission are sorted by cost per test, with the most recent test date noted.
PHLEBOTOMY BLOOD LOSS
IllumiCare uses a patent-pending method for estimating phlebotomy blood loss (ml) by day of length of stay. This reinforces that labs have both human and economic cost.
PROBABILITY OF A LAB-INDUCED ANEMIA
We provide clinicians with a probability of hospital-acquired anemia associated with phlebotomy blood loss. Blood transfusions are expensive for the hospital and potentially problematic for patients.
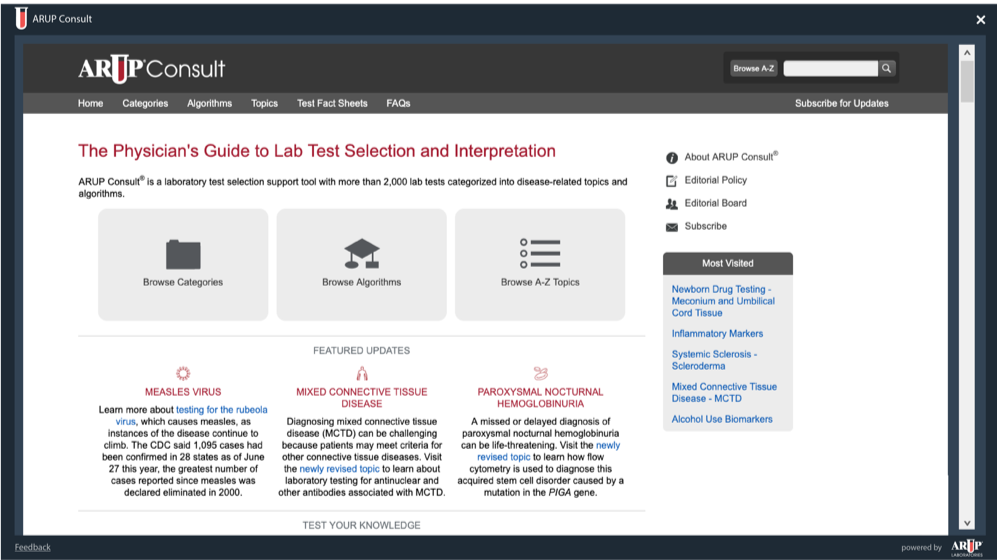
What is ARUP Consult?
ARUP Consult is a web-based laboratory test selection tool that provides point-of-care diagnostic and interpretive information for clinicians. ARUP Consult assists providers with test selection and interpretation among nearly 300 diseases and provides clinical background and diagnostic information. The content is expert-authored by ARUP and University of Utah, congruent with the latest medical guidelines and literature.
When should I use ARUP Consult?
ARUP Consult can be used to ensure providers are utilizing the latest best practices when they suspect a nuanced disease. Searching ARUP’s extensive database will enhance the providers knowledge and ensure they are utilizing the most up to date clinical practice to care for their patients.
Why doesn’t ARUP Consult contain information on all diseases?
ARUP Consult is a lab focused tool that aids in the clinical diagnosis of disease. It is not a replacement for broader content providers, rather, it narrows the scope of information and provides it in an easily digestible format for providers at the bedside.
How can I contact ARUP if I have questions about their recommendations?
Please contact ARUP at arupconsult@aruplab.com if you have questions or suggestions specific to their content.
-
Overview
-
Screenshot
-
Video
PATIENT SPECIFIC OBS CALCULATION
If a patient is on observation status, a timer will appear in the Smart Ribbon. The value represents the amount of time the patient has been on obs status. The numerical value will turn red after the patient exceeds the amount of time determined by your health system. The status will be displayed by a key performance indicator on the Ribbon icon. The icon will be the blue clock if the patient has not been on obs status longer than the limit set by the health system, otherwise it will be a red alert circle.
HOW IS OBS TIME CALCULATED?
The observation timer shows the current time a patient has been in an observation status. This is based upon the provider order to place them into the observation status.
WHY IS OBS TIME RED?
After 24 hours the Obs timer turns red to indicate that the patient is nearing the Two Midnight Rule. This is a visual reminder of the duration of time they have spent in that status.
-
Overview
-
Screenshot
-
Video
HIGH PRIORITY CLINICAL ANNOUNCEMENTS
Announcements are high priority clinical posts that may be relevant to specific facilities within your health system or relevant to your health system as a whole. New and past announcements are displayed on the home screen when you first open the app.
- Administrators may create, edit, save drafts, delete, and recover any announcements within their health system
- Calculated on every med, lab and radiology order
- Save as a 'Draft' and post at a later time
- Admins can edit already posted announcements
- Announcements appear on the ribbon with an illumination
- Post to individual regions within your health system


IT'S A PLATFORM TO DO SO MUCH MORE
As an EMR-agnostic platform of apps that automatically appears on the same screen and with patient context, it gives power back to clinicians to control their workflows, improve cost/quality and bring some joy back to clinical practice.



