Nudging and Reinforcement Increases Risk Capture and Quality Measures
Leaving Money on the Table
Medicare Advantage plans and Accountable Care Organizations, along with their respective network providers, can face significant lost revenue due to care and coding gaps in their member populations. For example, in 2021, Medicare Advantage plans with a 4-star or better rating received an average bonus of between $174-$521 per member.1 On the risk capture side, it has been estimated that for each 0.1 increase in risk score, a Medicare Advantage plan’s profits increase about 25 percent.2
Given the economic incentives at the plan level, many plans have a quality and risk capture incentive program for their provider community. For primary care providers, uncaptured risk codes can result in thousands of dollars in lost incentive payments offered by the network sponsor for submitting patient health risk assessments (HRA) and/or appropriately documenting chronic conditions in a given year. Providers can also receive cash incentives based on their composite quality star rating. The more care gaps closed, the higher the provider’s star rating, resulting in a higher quality bonus.
The common thread that runs through all incentive payments is the dependence of plans on primary care providers to close care and coding gaps in a timely and appropriate manner. As a result, they have to be able to influence the primary care providers in their networks where and when care is actually being delivered: in the provider’s office, at the point of care.
Research Highlights
An EMR-agnostic system of “nudging” primary care providers (and their staff) at point of care with care and coding gap information and then reinforcing that process with analytics on utilization and efficacy caused substantial increases in gap closure in a Medicare Advantage plan and an ACO.
- A large Medicare Advantage plan that focused on quality measures saw a 342% net increase in network providers who achieved a 4+ star quality rating.
- A statewide ACO increased HCC recapture rates by 25%.
These results show how multiple obstacles to reaching providers in a timely and relevant manner can be overcome through the application of non-intrusive technology that works seamlessly with a practice’s electronic medical record.
The Last Mile Fallacy
The promise of “interoperability” has been such a pervasive mirage that we have been lulled into believing that delivering content to the point of care (the so-called “last mile” of connectivity) is an end unto itself. It is not. Data delivery is only useful if it leads to behavior change. Simply cramming more data into an electronic medical record (EMR) does not magically get one the desired end result.
Behavior change requires (1) content delivery in a way that attracts attention without aggravation, (2) reinforcement through an ongoing focus on utilization and outcomes data and (3) the delivery and transparency of those measurables back to the provider community. That virtuous cycle is not only possible, but already in practice and producing positive results.
The Many EMR Conundrum
It’s not uncommon for Medicare Advantage plans and Accountable Care Organizations (ACO) to have members attributed to hundreds or thousands of primary care providers using many different EMR brands, with multiple versions. Using a Medicare Advantage plan that participated in this report as an example, even limiting to only those practices with 100 or more attributed members, it would still result in 18 separate EMR brands in use across those practices.
What is needed is an EMR-agnostic tool that requires no separate login, patient lookup, or EMR integration, and places care and coding gap requirements and information from the plan in front of primary care physicians during their normal workflow.
“Nudging” in Provider Workflow
 The IllumiCare Smart Ribbon® (“Ribbon”) is an EMR-agnostic tool that can be implemented at medical practices and IDNs painlessly and be proliferated across many practices quickly. It requires no EMR integration. It can be placed on any or all workstations at a medical practice (or within a virtualized desktop, as is common at larger entities). Users may include providers, APPs, nurses and support staff.
The IllumiCare Smart Ribbon® (“Ribbon”) is an EMR-agnostic tool that can be implemented at medical practices and IDNs painlessly and be proliferated across many practices quickly. It requires no EMR integration. It can be placed on any or all workstations at a medical practice (or within a virtualized desktop, as is common at larger entities). Users may include providers, APPs, nurses and support staff.
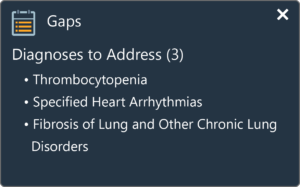
The Ribbon is a separate application that auto-starts upon login and simply runs in the background. If the user navigates to the EMR and to a specific patient’s record, and that patient also happens to be a member of a health plan from which IllumiCare has obtained gaps data, a “nudge” appears on the screen (see picture above). Much like a system notification about receiving a new email, the Ribbon uses motion to capture attention, but does not obstruct the user from their work. Today, more than 72,000 clinicians use it in their workflow. It has withstood the test of time and physician scrutiny.
If the user wishes to see more information about the member or access bi-directional functionality (e.g., HRA completion, diagnosis disputes, health maintenance signup, etc.), they click on the nudge or the Ribbon icon in the taskbar, which “opens the app.” (See a video of how this works here: https://illumicare.com/gaps-app/.) While the Ribbon is a common framework to deliver payer data to point of care, it is also a malleable tool, which allows each plan to use different “widgets” that relate to its own initiatives and data gathering needs.
Implementing Across a Diverse Provider Network
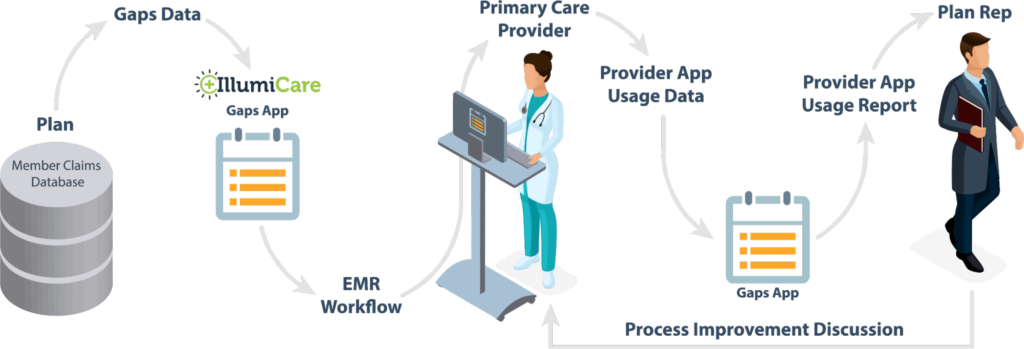
IllumiCare has worked with multiple health plans to implement the Ribbon in their provider network. Most plans span hundreds to thousands of providers in their network. In each case, the plan used several factors in considering which practices to invite, including number of attributed members, current quality measures and current risk capture performance. For each payer, IllumiCare created invitation materials to facilitate provider adoption (see, e.g., https://illumicare.com/bcbsal/). IllumiCare held informational sessions and one-on-one meetings with the designated practices. Ninety-nine percent (99%) of all invited practices agreed to the implementation, which was free to the practices. Smaller practices were usually implemented in 1-2 hours. Larger IDNs generally took several months to navigate their technical review and change management processes. When implementations began, the plan commenced sending member and gap data to IllumiCare via flat file or API. Then, within an implemented practice, when a user viewed the plan’s member in their EMR, they would be nudged with the plan’s data on care and coding gaps (as well as other functionality).
Post-Implementation: Reinforcement
As the old adage goes, “What gets measured gets done.” One of the key benefits to the Ribbon being a separate application is that interaction with it generates an audit trail. On a weekly or monthly basis (at the preference of the plans), IllumiCare fed back to the plans data about who used the Ribbon, how it was used and what the gap closure rates were for users versus non-users. In most cases, these data were summarized inan “executive report” to the plans, but also separate, practice-specific reports were generated and shared with the provider relations teams at the plans. In each case, what developed was a positive cycle of providers viewing and acting on the plans’ data about the member, the plans receiving data about user actions and efficacy, and then plans’ representatives following up with the practice to show them their reports and either thank them for their engagement or spur on additional engagement when necessary. This “two-sided transparency” was seen as a critical component of the initiative.
Results
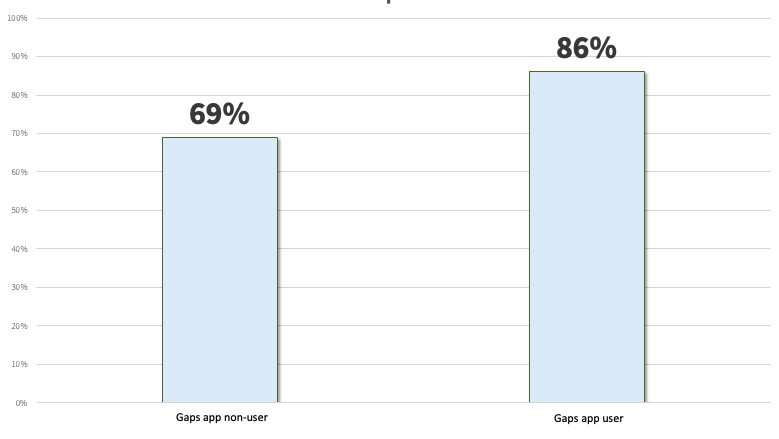
Deploying the Ribbon to a provider network improves both quality measures and risk capture. From the quality measure perspective, a study was conducted from March to September 2022, to track user and non-user behaviors of primary care providers who had access to member care gaps data provided by a Medicare Advantage plan via the Ribbon. At the start, 7% of all new Ribbon users were rated 4+ stars, while 10% of the non-users (other primary care doctors in the same network) were 4+ stars. Over the seven-month period, the Ribbon users went from 7% to 31% (an increase of 342%) achieving 4+ stars, while the non-users went from 10% to 20%, as shown in the chart below. [Note: an increase in star rating over the course of a calendar year is expected, given that some quality measures reset on a yearly basis and can be closed when the patient has an annual wellness visit; what is noteworthy here is the relative increase of users vs. non-users.]
Care Gap Closure Tracking Chart3
 From a risk capture perspective, an ACO that deployed the Ribbon to their providers saw that when a provider was nudged and opened the app, they realized an increase of 25% in HCC recapture rates, as compared to those providers who didn’t open it.
From a risk capture perspective, an ACO that deployed the Ribbon to their providers saw that when a provider was nudged and opened the app, they realized an increase of 25% in HCC recapture rates, as compared to those providers who didn’t open it.
The monthly value, classified as “ribbon user” or “non-ribbon user,” is the count of National Provider Identifiers (NPI) greater than or equal to 4 stars for that given period divided by the total number of NPIs. A provider is calculated as being a 4-star provider by meeting certain cut points on quality measures. CMS has cut points for the measures they reimburse to the payers and payers have their own cut points used for the provider incentives for certain measures.
Chart Formula
HCC Recapture Rate4
 It’s About Real Behavior Change…Not Just Delivering Data
It’s About Real Behavior Change…Not Just Delivering Data
It’s no longer enough to simply enable last mile connectivity. It’s a necessary step in the process, but as the study results show, the real value is found in facilitating lasting behavior change among network providers. One of the key benefits of an EMR-agnostic tool such as the Ribbon is the ability to not only deliver timely gaps data to providers, but to have full insight into which providers actually use it, when they use it, and what they do with it. Doing so creates an enforcement loop that didn’t previously exist. These insights enable network reps who work with providers to change the conversation from broad outcomes to specific process improvements for increasing their risk capture and quality measures. For the first time it makes the gap closing process manageable and enforceable.
1 KFF: Spending on Medicare Advantage Quality Bonus Program Payment Reached $10 Billion in 2022
2 Medicare Advantage, Direct Contracting, And The Medicare ‘Money Machine,’ Part 1, HealthAffairs 2022
3 IllumiCare 2022
4 IllumiCare 2022